GLP-1 Therapies: How These Revolutionary Medications Are Reshaping Healthcare Costs
Key Takeaways
- GLP-1 medications show remarkable efficacy for multiple chronic conditions
- Current U.S. list prices range from $1,000-$1,500 monthly
- These therapies are creating both opportunities and challenges for healthcare payors
- Long-term benefits must be weighed against immediate costs
In the ever-evolving healthcare landscape, few breakthroughs have caused as much stir as GLP-1 receptor agonists (GLP-1 RAs). Originally developed for type 2 diabetes, these medications have shown remarkable efficacy in not only improving blood sugar control but also addressing obesity, metabolic-associated steatotic liver disease (MASLD), chronic kidney disease (CKD), and reducing cardiovascular disease. With their potential to prevent and manage many chronic health conditions, GLP-1s are poised to disrupt the healthcare system in unprecedented ways. However, with this disruption comes a significant dilemma: How can payors afford these life-changing yet costly medications in the face of escalating healthcare expenses?
GLP-1s: Effective Preventive Treatment for Chronic Diseases
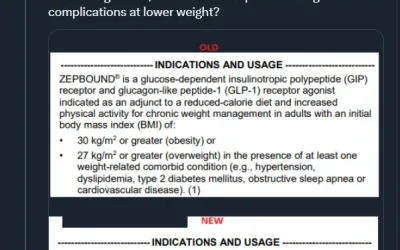
Chronic diseases — such as diabetes, cardiovascular disease, CKD, and obesity — have long been significant drivers of healthcare costs in the US. Traditionally, treatment has been reactive, focused on managing symptoms after the diseases have already taken hold. This approach developed primarily due to a healthcare system incentivizing managing disease rather than preventing it. GLP-1 receptor agonists, like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound), are changing this paradigm. GLP-1s offer a preventive approach by targeting key factors earlier in disease progression, such as insulin resistance, appetite dysfunction, inflammation, and excess dysfunctional fat, addressing the root causes of many modern chronic health epidemics.
Why Are They So Impactful? GLP-1s Go Further Upstream
Multiple studies highlight the efficacy of GLP-1s in weight management and cardiovascular risk reduction. For instance, the SUSTAIN-6 trial demonstrated that semaglutide reduced the risk of major cardiovascular events by 26% in patients with type 2 diabetes. This finding was further supported by the SELECT trial, which showed a 20% reduction in 3-point major adverse cardiovascular events (MACE) in people with obesity but without diabetes. The benefits of these medications extend to the kidneys, liver, and potentially the brain, immune system, and gut. These wide-ranging effects are predictable based on how the drugs work, offering significant promise for comprehensive chronic disease management.
Source: https://www.nature.com/articles/d41586-024-03074-1
The Price Problem: How Much Can Healthcare Afford?
Despite their promise, the cost of GLP-1 therapies presents a significant obstacle. In the U.S., the list price of these medications can range from $1,000 to $1,500 per month. These costs are particularly burdensome considering that chronic conditions like obesity and diabetes often require long-term or even lifetime treatment. While manufacturers negotiate rebates with pharmacy benefit managers (PBMs), which can reduce the net cost, the gross-to-net pricing remains opaque. This lack of transparency leaves patients and payors uncertain about the actual cost of GLP-1 therapies.
While payors may benefit from lower net costs after rebates, the overall expense of GLP-1s remains significant compared to other obesity interventions. This challenge is exacerbated by the increasing demand for these medications, particularly as more patients seek treatment for obesity and related disorders. Even with rebates, the net cost to payors and employers remains substantial. As the use of GLP-1s for obesity management increases, spending growth could become unsustainable, adding to the financial strain in a healthcare system already plagued by inefficiencies.
The Existential Crisis for Payors
The dilemma for insurers is clear: They cannot afford GLP-1 therapies, but they also cannot afford not to cover them. On one hand, the clinical benefits are undeniable — improved metabolic health, reduced cardiovascular risk, fewer hospitalizations, and lower long-term societal costs. Employers are particularly interested, as these therapies can enhance workplace productivity and reduce absenteeism. A joint survey by Ro and the Obesity Action Coalition (OAC) showed growing employee demand for obesity treatments while employers grapple with the potential benefits of offering such coverage.
On the other hand, the short-term costs of covering GLP-1s are staggering, especially in the U.S. healthcare system, which is notorious for its inefficiency and high administrative costs. Payors, both public and private, must justify spending tens of thousands of dollars per patient annually on these medications amid rising prescription drug costs and an aging population. The systemic tension between the high upfront costs and long-term benefits of GLP-1s is pushing the healthcare system toward a tipping point, exposing its unsustainable cost structure.

Source: https://www.wtwco.com/en-us/insights/2024/02/glp-1-drugs-implications-for-employer-health-plans
The Coming Reckoning: Addressing Systemic Costs
The rise of GLP-1 therapies represents more than just a medical breakthrough — it is a tipping point that will force payors, healthcare providers, and policymakers to address broader issues within the healthcare system. For years, the U.S. healthcare system has been weighed down by inefficiencies, excessive administrative overhead, and misaligned incentives among providers, insurers, and pharmaceutical companies. GLP-1s may be the catalyst for a long-overdue reckoning with these inefficiencies.
Payors will need to find ways to balance the cost of preventive treatments like GLP-1s with their long-term savings in reducing hospitalizations and managing chronic diseases. Studies suggest that GLP-1 therapies could generate significant savings by lowering direct medical costs associated with obesity and reducing societal costs. Achieving this balance will require a shift in how healthcare costs are viewed — not just short-term expenses but long-term outcomes and value-based care.
The Path Forward
Navigating this complex landscape will require collaboration among healthcare stakeholders to develop new care models and payment structures that prioritize preventive treatments and value-based care. Policymakers should push for greater transparency in drug pricing, especially around gross-to-net costs, to prevent inefficiencies and excessive markups from straining the system.
Ultimately, the future of GLP-1 therapies depends on adapting the healthcare system to support preventive medicine while controlling costs. This will involve difficult decisions and challenging conversations, but the potential rewards — both in terms of patient outcomes and cost savings — are too significant to ignore.
Conclusion
GLP-1s represent a groundbreaking solution to some of healthcare’s biggest challenges, but they also highlight the need for deep structural reform. As the healthcare system grapples with the costs of these life-changing medications, it must also seize the opportunity to address its inefficiencies. The clock is ticking, and the time for meaningful change is now.
Ready to learn more about medical obesity care? Schedule a consultation with an Accomplish Health physician today.
Disclosures:
- Cofounder and CMO of Accomplish Health: a comprehensive virtual obesity medicine platform for patients, providers, and payors
- Consultancy: Elo Health, Gelesis, and Novo Nordisk